Enterotoxemia, or anaerobic dysentery of sheep, is a toxic infection caused by anaerobic bacteria. The disease manifests itself as serious nervous disorders, hemorrhagic enteritis, digestive disorders, and general intoxication of the body. Sheep of any breed and age group are susceptible to enterotoxemia. If treatment is not started in time, the infection inevitably leads to the death of farm animals.
Pathogen and causes of the disease
Enterotoxemia in sheep is caused by rod-shaped, gram-negative anaerobic bacteria Clostridium perfringens types C, D, and less commonly A.Clostridia produce toxins. In the external environment they form capsules. On nutrient media, after penetration into the body of animals, spores form. Bacteria in spore forms in soils remain virulent for up to 3-4 years. Withstand heating up to 85 degrees, boiling for 13-15 minutes. The death of clostridia is caused by a 5% formaldehyde solution and bleach.
The main sources of enterotoxemia are sick individuals, latent (hidden) carriers, and recovered animals. Transmission factors include bedding, animal care equipment, and household items contaminated with bacteria.
Important! Infection of sheep with anaerobic dysentery occurs through contact, nutritional means.
Causes of enterotoxemia in sheep:
- unfavorable living conditions (high humidity, lack of ventilation, non-compliance with temperature conditions);
- feeding rotten, moldy, low-quality feed, wet hay;
- a sharp transition from one diet to another;
- eating large amounts of wet or young juicy grass;
- the predominance of concentrated feed in the diet;
- early weaning of lambs;
- autoimmune diseases;
- protein, mineral deficiency, vitamin deficiencies;
- helminthiases (helminthic infestations).
The development of infection in sheep is facilitated by acute and chronic gastrointestinal pathologies, secretory dysfunction, as well as a sharp transition from stall to pasture housing. Newborn lambs become infected from lactating lambs.
Signs and symptoms
Once in the body of animals, clostridia produce toxins and actively multiply in the tissue cells of the digestive tract. The waste products of bacteria lead to the formation of ulcers, erosions, necrotic lesions, and internal hemorrhages.The liver, intestinal mucosa, serous membranes, and vascular endothelium are affected. Their permeability increases. Secretory function, intestinal motility, and the functioning of internal organs are disrupted.
Important! Enterotoxemia in sheep is most often diagnosed by veterinarians in the spring and summer, less often in autumn and winter. The infection is seasonal.
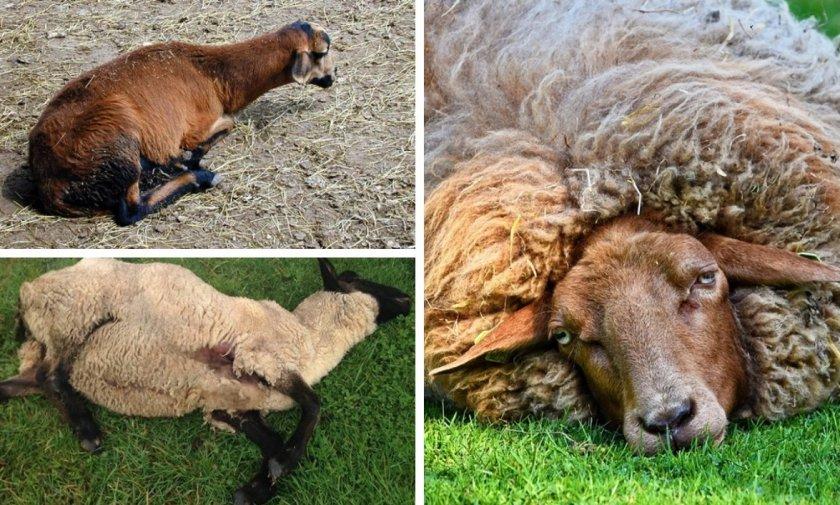
Main symptoms and manifestations of enterotoxemia:
- refusal of food;
- sudden weight loss;
- restless behavior followed by depression;
- disruption of growth and development of young animals;
- change in heart rate;
- sudden loss of coordination;
- inadequate response to external stimuli;
- loss of consciousness;
- increase in temperature by 1-3 degrees, fever;
- grinding of teeth;
- nervous disorders;
- salivation, accumulation of foam in the corners of the mouth;
- intestinal disorders;
- profuse diarrhea;
- pallor, cyanosis of mucous membranes;
- respiratory dysfunction;
- muscle spasms, cramps.
In newborn lambs, individuals aged from 2-3 weeks to one month, enterotoxemia occurs in an acute form. The first symptoms appear 3-5 hours after infection. In adult animals, an acute, hyperacute, and less often chronic course of the disease is noted. The first signs of infection are noticeable 3-4 days after infection. Death occurs on 7-10 days.
In some cases, enterotoxemia develops suddenly in fattening sheep. Animals die without any manifestations of the disease. The death is caused by severe intoxication, dehydration, and paralysis of the respiratory system. Mortality from enterotoxemia occurs in 85-95% of cases.
Diagnostic measures
When making a diagnosis, anamnesis data, external manifestations, and the epizootological situation in the region regarding enterotoxemia are taken into account.A more clear picture can be obtained after laboratory tests and pathological changes. Differential diagnosis is carried out, since the symptoms of enterotoxemia are similar to peptic ulcers, intestinal infections, bradsitis, and listeriosis.
How to treat infectious enterotoxemia
In the acute, hyperacute form of enterotoxemia in sheep, treatment is difficult. If the disease is chronic, veterinarians use complex antibiotics, tetracycline antibacterial agents for intramuscular injection, and sulfonamide drugs. Duration of therapy is 4-5 days. The dosage of medications is selected individually, depending on the age and general condition of the animals. Good results are observed after therapy with bivalent hyperimmune serums, which are effective against anaerobic bacteria.
Important! Infected animals are placed in quarantine zones and isolated from healthy sheep. Healthy sheep that have been in contact with sick individuals are treated with antitoxic serum to prevent infection.
Additionally, immunostimulants, probiotics, and symptomatic medications are prescribed to normalize digestion, the functioning of internal organs, and eliminate clinical manifestations. During treatment, it is necessary to carry out a number of disinfecting measures, normalize living conditions, and eliminate factors contributing to the further spread of infection. After completion of therapy, a comprehensive examination of recovered individuals is carried out. The material is sent to laboratories for bacteriological research.
What could be the consequences?
Anaerobic dysentery can cause disruption of digestive processes and provoke chronic cardiovascular and nervous pathologies. Young animals that have recovered from the disease are retarded in growth and development and gain weight poorly.
Important! If treatment is not started, anaerobic dysentery is fatal in 100% of cases.
Sheep that have recovered from the disease develop specific immunity that lasts up to 12-15 months.
Prevention
In livestock farms located in regions with unfavorable conditions for enterotoxemia, routine comprehensive vaccination against infectious diseases is mandatory. The vaccination schedule is set by the veterinarian. To prevent sheep from becoming infected with anaerobic dysentery, it is necessary to monitor the quality of feed, systematically disinfect equipment, and periodically change bedding. It is necessary to monitor the microclimate parameters in premises with animals.
To increase the resistance and immune potential of sheep, diets are supplemented with vitamin and mineral premixes and additives. The export of sheep from farms unaffected by this infection, forced slaughter, regrouping of animals within livestock complexes, and skinning of sick animals are prohibited. The corpses of sheep and lambs that died from enterotoxemia are subject to mandatory disposal.